Volume 11, Issue 1 (Winter 2022)
J Occup Health Epidemiol 2022, 11(1): 48-66 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rezaei-Hachesu V, Naderyan Fe’li S, Maajani K, Golbabaei F. The Global Prevalence of Anxiety, Depression, and Insomnia among Healthcare Workers during the Covid-19 Pandemic: A Systematic Review and Meta-Analysis. J Occup Health Epidemiol 2022; 11 (1) :48-66
URL: http://johe.rums.ac.ir/article-1-484-en.html
URL: http://johe.rums.ac.ir/article-1-484-en.html
Related article in
Google Scholar
Google Scholar
Similar articles
1- PhD Candidate in Occupational Health Engineering, Dept, of Occupational Health, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran.
2- PhD Candidate in Epidemiology, Dept. of Epidemiology and Biostatistics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran.
3- Instructor of Occupational Health Engineering, Dept. of Occupational Health Engineering, School of Public Health, North Khorasan University of Medical Sciences, Bojnurd, Iran.
4- Professor of Occupational Health Engineering, Dept, of Occupational Health, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. ,fgolbabaei@tums.ac.ir
2- PhD Candidate in Epidemiology, Dept. of Epidemiology and Biostatistics, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran.
3- Instructor of Occupational Health Engineering, Dept. of Occupational Health Engineering, School of Public Health, North Khorasan University of Medical Sciences, Bojnurd, Iran.
4- Professor of Occupational Health Engineering, Dept, of Occupational Health, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. ,
Article history


Received: 2021/10/22
Accepted: 2022/01/4
ePublished: 2022/03/25
Accepted: 2022/01/4
ePublished: 2022/03/25
Subject:
Occupational Health
Keywords: COVID-19 [MeSH], Anxiety [MeSH], Depression [MeSH], Insomnia [MeSH], Health Personnel [MeSH]
Full-Text [PDF 711 kb]
(1407 Downloads)
| Abstract (HTML) (5463 Views)
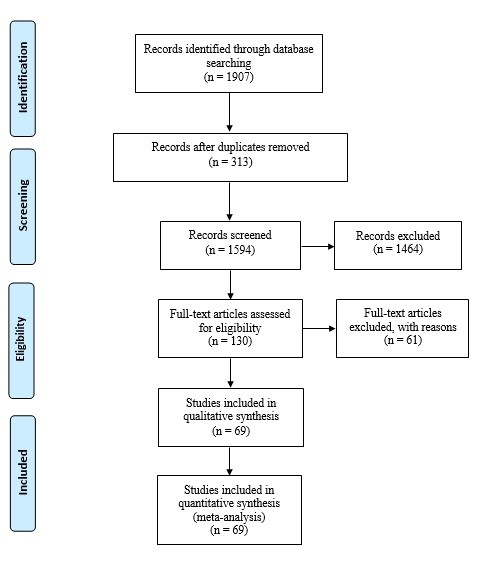
Fig. 1. PRISMA flowchart of different phases in searching the relevant publications

Fig. 2. Forest plot of pooled prevalence of anxiety in healthcare workers
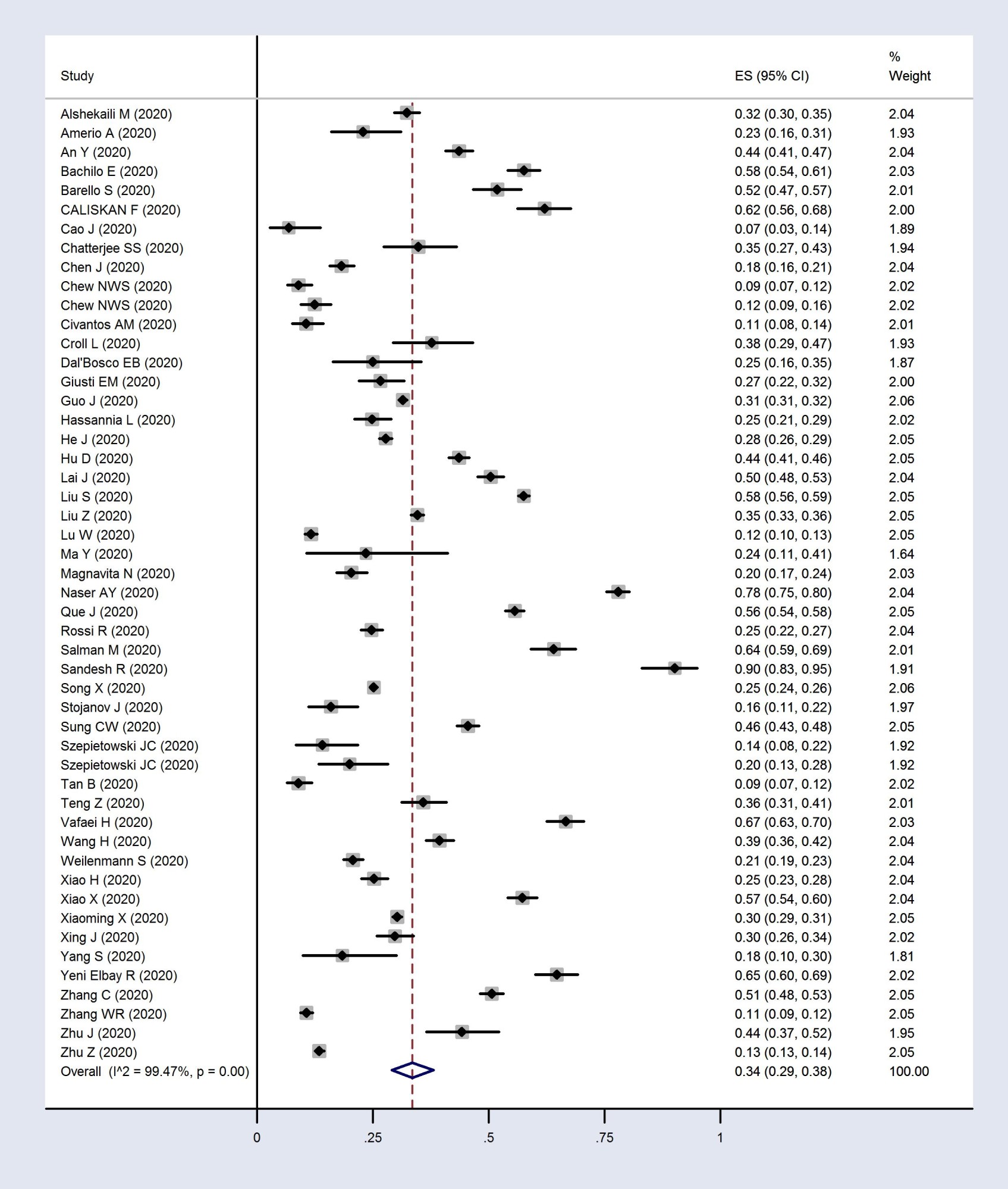
Fig. 3. Forest plot of pooled prevalence of depression in healthcare workers

Fig. 4. Forest plot of pooled prevalence of insomnia in healthcare workers
Table 3. Meta-regression analysis for the effect of the suspected variables on the pooled prevalence of anxiety, depression, insomnia in medical staff
Discussion
This systematic review and meta-analysis showed a high prevalence of psychiatric disorders among healthcare personnel during the COVID-19 crisis. Based on its results, the pooled prevalence rates of anxiety, depression, and insomnia were 37%, 34%, and 39%, respectively.
The findings showed that a high proportion of HCWs experienced considerable mental health disorders during the COVID-19 pandemic. This work, similar to many previous ones, implies the importance and urgency of attention to the mental health of medical staff.
Compared with the original systematic review (87), a higher prevalence of mental disorders was found (23.21% vs. 37% for anxiety, 22.8% vs. 34% for depression, 34.32% vs. 39% for insomnia in the original and present review, respectively). The pandemic of the new coronavirus is associated with many potential stressors that can lead to psychological problems and adverse consequences, especially among medical staff directly dealing with the crisis. Therefore, a high burden of mental health disorders is expected among them. In addition, the current review includes studies conducted over a longer period from the beginning of the epidemic. The fact that some countries have failed to control the disease despite many efforts and the number of disease cases is increasing worldwide may have caused more anxiety and fear among the medical staff.
Anxiety related to COVID-19: Anxiety disorders are defined as excess worries and fears that debilitate and cause a loss of quality of life [84, 85]. The present review findings showed that a large number of HCWs felt anxious about the prevalence of the COVID-19 pandemic. Anxiety in healthcare providers during the COVID-19 pandemic can be caused by factors such as shortage of PPE, fear of contact with infected people, getting infected and spreading the disease to families and friends, and fear of death [86, 87]. Healthcare professionals might be at a higher risk for developing anxiety disorder because of the emerging and life-threatening nature of the new coronavirus, increased workload and fatigue, lack of self-efficacy, and insufficiency of social support [88]. In this regard, social and economic consequences can result in more concerns [86]. In a survey conducted in Wuhan City in China, 63.2% and 28.0% of the frontline nurses reported moderate and severe levels of fear, respectively. Additionally, 11.0% and 3.3% of these nurses had moderate and severe anxiety levels [88].
In this review, the prevalence of anxiety was higher in female HCWs than in males (39% vs. 30%). In the same line, a previous study indicated that the Self-Rating Anxiety Scale for female nurses was higher than for males, indicating a higher level of anxiety among females [88]. A previous systematic review and meta-analysis among HCWs showed anxiety disorder to be more prevalent in females than males (29.06% vs. 20.92%, respectively) [89]. Nurses working in different units also noted that anxiety was more likely among women than men [90, 91]. Sex differences in the occurrence of anxiety can be due to genetic, neurodevelopmental, environmental, and neurobiological factors. Brain structural and functional differences, as well as hormonal differences between men and women, may have a critical role in the neurobiology of anxiety disorders. There are differences between the brain of men and women in areas dependent on anxiety, including the prefrontal cortex, hippocampus, and extended amygdala complex. Moreover, estrogen and progesterone, as female reproductive hormones, can play a key role in the neurobiology of anxiety disorder. Periodic fluctuations in these hormones throughout a woman's life can also precipitate Hypothalamic-Pituitary-Adrenal axis responses. These large fluctuations in sex hormone levels may contribute to changes in the severity of anxiety symptoms at different stages of reproduction in women [91]. Thus, female medical staff are assumed to be a more vulnerable group affected more severally by anxiety; accordingly, this disorder may be a much more important issue in women.
Depressive disorders: Depression is characterized by slow psychic processes, depressed and/or irritable mood, reduced energy, sad feelings, disinterest, apathy or psychomotor agitation, difficulty in concentrating, negative thoughts, loss of planning capacity, and altered judgment of the situation [36].
During the COVID-19 pandemic, a high frequency of depressive cases was reported among HCWs worldwide. For example, in a systematic review of 59 studies, the prevalence of depression was reported within the range of 5% to 51% [92]. In another systematic review and meta-analysis, the pooled prevalence of depression was 36% among the health professionals, based on a random-effects model (95%CI: 0.19 to 0.58) [93].
Furthermore, witnessing the suffering of patients with COVID-19 and being incapable of saving the lives of some patients make the medical staff upset. In the long run, this issue can make HCWs prone to depression and other psychological diseases since depression is often comorbid with anxiety [94]. Consequently, causative factors of anxiety in HCWs, such as insufficient understanding of the disease, lack of prevention knowledge, fear of getting infected, and transmission of the infection to family members, predispose the staff to depression.
In a survey in China, the researchers found that insufficient PPE and a history of contact with diagnosed COVID-19 patients were two independent risk factors for developing depression among HCWs. In this regard, having no contact with the COVID-19 patients was found as a protective factor [76]. In a cross-sectional survey in China, gender (male) was considered a protective factor for depression among doctors [82]. This finding was consistent with the present review results; the prevalence of depression in female HCWs was higher than the males (36% vs. 32%).
Given the confirmed findings that depression is generally more common in females [95, 96], authorities are required to take measures to prevent and control depression in female HCWs.
Insomnia related to COVID-19: Insomnia disorder refers to the difficulty in falling or staying asleep, poor sleep quality, or less sleep duration. This disorder often co-occurs with other mental illnesses, such as depression. Insomnia also may lead to physical and mental morbidities and reduce the quality of life [97].
In the critical situation caused by the COVID-19 outbreak, HCWs experience different levels of insomnia [92, 98]. In the present review, a high prevalence of insomnia was reported among the medical staff. This disorder was especially more common among nurses and women. These findings were in line with a previous systematic review and meta-analysis indicating that the pooled prevalence of sleep disturbances was significantly lower among male HCWs than the females (33.8% vs. 46.4% p < 0.001). Additionally, the prevalence of sleep disturbances among nurses was higher than among doctors [99].
In general, gonadal steroid effects are a potential reason for the increased prevalence of insomnia among females compared with males [100]. Considering the direct association of depression with insomnia and the high prevalence of depression among women in this study, a high frequency of insomnia is also expected.
Nurses responsible for taking care of patients with COVID-19 are at a higher risk of infection because they are in close and frequent contact with such patients and should work longer hours than usual [6]. Consequently, such a situation may play a role in causing insomnia. Furthermore, anxiety, depression, and insomnia are closely related to their risk factors. In a study carried out among the medical health workers in China, the history of organic diseases, residence in rural areas, risk of contact with COVID-19 patients, and female gender were among the independent risk factors for insomnia, anxiety, and depression [81]. Shift working, increased workload, education level, and worrying about getting infection were also among the other risk factors for developing insomnia [98, 101].
The strength of this systematic review is that it includes a wide range of published articles covering a large sample size. In the case of the study limitations, the following issues can be mentioned: an inherent and considerable heterogeneity was observed in the pooled prevalence of anxiety, depression, and insomnia. Hence, a random-effects model was applied to calculate the pooled prevalence of outcomes. Subsequently, subgroup analysis and a meta-regression model were conducted. Moreover, since the included articles used different tools to measure the participants' mental health disorders, the pooled prevalence of outcomes may be questionable. In this vein, a subgroup analysis was conducted based on the assessment tools. Another limitation of this review was the low quality of some included studies.
To the best of the authors' knowledge, this study is the most comprehensive systematic review and meta-analysis of primary studies on the prevalence of anxiety, depression, and insomnia in HCWs during the Coronavirus pandemic. However, one of the limitations of this study was the unavailability of the full text of some articles, ultimately leading to the exclusion of such articles from the meta-analysis. In addition, the low quality of some included articles was another limitation.
Conclusion
The findings indicate a high impact of the COVID-19 pandemic on the mental health of HCWs involved in the crisis in various territories and occupations among both genders. The medical staff's mental health is as crucial as their physical health. Moreover, mental health is important not only for the medical professionals' well-being but also for their work efficacy, improving the quality of medical services and patients' health. To reduce the staff fear of the new epidemic, adequate training is required to shed light on the disease's nature and supply adequate resources such as PPE. Furthermore, special attention should be paid to providing HCWs with appropriate levels of social and psychosocial support. In order to improve sleep quality among the staff, the following measures can be taken: decreasing anxiety and depression, applying relaxation techniques, using medications, and providing an opportunity for adequate rest.
Acknowledgement
We appreciate Hamide Behroueian for editing the manuscript in terms of its language and readability.
Conflict of interest: None declared.
Full-Text: (885 Views)
Introduction
On December 27, 2019, the World Health Organization office in China reported cases of pneumonia from the live animal market in Wuhan city, the capital of Hubei province [1]. On January 7, 2020, the etiologic agent of this pneumonia was identified as the "new coronavirus" (2019-ncoV), not previously seen in humans. The disease caused by 2019-ncoV was later named Coronavirus 2019 (COVID-2019), which was renamed SARS-CoV-2 considering its close resemblance to SARS-COV [2].
At the moment, many countries worldwide are facing the COVID-19 pandemic. Although limiting the crisis through a lockdown and widespread vaccination is important to reduce the virus's physical impacts, the pandemic's mental health consequences seem to be another substantial issue [3,4].
Health care workers (HCWs), who are directly involved in diagnosing, treating, and curing patients with COVID-19, are at risk for physical and mental problems. The HCWs are exposed to a heavy psychological burden due to the increasing number of suspected cases, overworking for long periods, lacking enough personal protective equipment, worrying about transmitting the disease to the family and friends, and lacking the required medications and sufficient support for all patients [5-8]. Since HCWs play a key role in controlling the epidemic and reducing the complications of the disease, maintaining their health is not only important from an individual point of view but also ensures the general public health. Previous studies have shown an increased prevalence of mental disorders among HCWs after initiating the Coronavirus pandemic. In a country-wide survey among HCWs conducted from March 2 to April 2, 2020, in China, the prevalence of depression and anxiety were 15.5% and 12.7%, respectively [9]. Moreover, the prevalence of depression and anxiety among HCWs during the COVID-19 pandemic was 28.1% and 33.1%, respectively, in a cross-sectional study in the UK [10].
At the beginning of this pandemic, all healthcare workers were under tremendous pressure. Excessive workload combined with fear of infection may cause mental disorders. The prevalence of mental disorders as an indicator of the imposed burden can show the importance of mental health in HCWs. On the other hand, the prevalence can vary over time with changes in factors such as better understanding of the disease and improvement in medical care facilities.
Differentiating short- and long-term impacts of the pandemic, in terms of time-horizon, on HCWs' mental health is necessary for policymaker guidance towards more evidence-based planning to overcome associated challenges. Thus, this systematic review and meta-analysis aimed to show the globally pooled prevalence of anxiety, depression, and insomnia among HCWs from a short-term perspective during the COVID-19 pandemic. To do so, individual studies conducted during the first 8 months after the onset of the pandemic were considered.
Materials and Methods
To conduct this systematic review and meta-analysis, PRISMA (Preferred Items for Reporting Systematic Reviews and Meta-Analyses) checklist was followed [11].
All relevant English articles on the prevalence of insomnia, anxiety, and depression among healthcare providers in dealing with COVID-19 were included in this review. Abstracts without full texts, editorials, case reports, and reviews were excluded from the study. Also, articles that did not use a valid questionnaire to measure anxiety, depression, and insomnia were excluded. Studies conducted on children, the general population, and hospitalized patients were excluded as well. Moreover, since the prevalence of an outcome in a case-control study cannot provide a good estimate in the reference population, such studies were also excluded.
To collect the data, two independent researchers searched databases of Web of Science, Scopus, Medline (PubMed), and Embase up to August 24, 2020. Moreover, preprint servers of medRxiv and SSRN were investigated. A search strategy was prepared using the combination of the following keywords: ("medical staff*" OR "Health Personnel" OR healthcare OR "Healthcare Worker*" OR "Health Care Provider*" OR "healthcare professional*") AND (COVID-19 OR "2019 novel coronavirus disease" OR "COVID-19 pandemic" OR "SARS-CoV-2 infection" OR "2019-nCoV infection" OR "coronavirus disease 2019" OR "severe acute respiratory syndrome coronavirus 2" OR 2019-nCoV OR "Wuhan coronavirus" OR SARS-CoV-2) AND (Depression OR "Depressive Symptom*" OR anxiety OR Nervousness OR insomnia OR "Sleep Initiation and Maintenance Disorders" OR "Early Awakening" OR "Sleep Initiation Dysfunction*" OR "mental health" OR psychological)
All identified studies were exported to the EndNote software (version X8, for Windows, Thomson Reuters, and Philadelphia, PA, USA). After removing the duplicates, two independent researchers evaluated titles and abstracts according to the study eligibility criteria. In the case of inconsistency between reviewers, a third reviewer assessed the eligibility criteria for the study to be included in the review.
Two independent researchers developed data extraction sheets to obtain relevant data, including the first author's name, publication date, occupation, study location, study design, sample size, response rate, age, and gender. The
prevalence of anxiety, depression, and insomnia, as well as outcome assessment methods and their cut-off points, were also collected. In the case of missing information, the necessary calculations were made.
The risk of bias in the primary studies was evaluated using the Newcastle-Ottawa quality assessment scale (NOS) for the case-control designs, and a customized version was developed for cross-sectional studies by two independent authors. The NOS is a star system developed to judge studies over three broad aspects: the selection of the study groups, the comparability of the groups, and the ascertainment of either exposure or outcome of interest. Each item on the scale is scored from one, which can be adapted to the specific topic of interest, to two. Thus, the maximum attainable stars (scores) for each study is nine, and studies with less than five stars indicate a high risk of bias [12].
In order to estimate the pooled prevalence of mental disorders among the medical staff during the COVID-19 pandemic within the 95% confidence interval (CI), the prevalence of anxiety, depression, and insomnia were examined in different articles from all over the world. Since CIs and standard errors (SEs) were not reported in some studies, the binomial distribution was applied to calculate them.
In the case of proportions near boundaries (in this instance, prevalence near 100% or zero), metan command was used to exclude the studies with such prevalence from the pooled estimate. Hence, the metaprop command was applied to estimate the exact binomial and score test based on CI for these proportions [13]. Also, the test at the 10% significant level (P<0.1) and the
test at the 10% significant level (P<0.1) and the  index were used to assess the between-study heterogeneity. According to the notable between-study heterogeneity, Der-Simonies and Laird random-effects models were used to calculate the pooled prevalence of anxiety, depression, and insomnia in medical staff [14].
index were used to assess the between-study heterogeneity. According to the notable between-study heterogeneity, Der-Simonies and Laird random-effects models were used to calculate the pooled prevalence of anxiety, depression, and insomnia in medical staff [14].
Further, the pooled prevalence of anxiety, depression, and insomnia was estimated in different subgroups based on the variables such as gender, occupation, and the assessment tool. In order to reduce the strata of occupations, three categories of doctors, nurses, and other occupations (including administrative staff, technicians, public health administrators, midwives, residents, or medical students) were considered.
Moreover, a meta-regression analysis was carried out based on gender, occupation, and country of the study to investigate the potential source of heterogeneity. The publication bias was not examined in this study. Given that the estimated pooled prevalence and the probability of proportion are always positive numbers, any probable asymmetry in the funnel plot is not due to the publication bias [15]. In order to perform all statistical analyses, STATA 11 (StataCorp, College Station, TX, USA) was used.
Results
After the initial search through international databases, 1,907 studies were retrieved, the results of which were screened. Finally, 69 articles were included in the systematic review and meta-analysis. Fig.1 illustrates the process of selecting the relevant studies.
The total sample size for 69 included studies consisted of 102,349 medical staff. A total of 26,272 staff were male and 74,807 were female. According to occupation, 25,601 individuals were doctors, 47,449 were nurses, and 17,676 had other occupations within the medical realm. The evaluated studies (n = 69) were conducted in China (n = 31), Italy (n =7), Iran (n =3), and Turkey (n =3). Furthermore, two studies were conducted in each of the following countries: Oman, the USA, and Pakistan. In the following countries, one study was carried out: Thailand, Russia, Brazil, Switzerland, Korea, Taiwan, Philippines, Israel, Jordan, United Arab Emirates, Poland, Ecuador, Nepal, Saudi Arabia, Singapore, India, and Serbia. Moreover, one study was conducted in 30 countries, and one study was performed in two countries. Characteristics of the included studies are summarized in Table 1.
Risk of bias within studies: The NOS results for each study are presented in Supplementary Table 1.
Forest plots of pooled prevalence of mental health disorders (anxiety, depression, and insomnia) are presented in Figs. 2 to 4. Anxiety prevalence was estimated in 61 studies. In the present meta-analysis, the pooled prevalence of anxiety was 37% (95% CI: 31 to 43%). Depression was investigated in 50 studies. The pooled prevalence of depression was 34% (95% CI: 29 to 38%). Insomnia was estimated in 10 studies. The pooled prevalence of insomnia was 39% (95% CI: 25 to 53%) (Table 2).
According to the results of the test and
test and  index, significant heterogeneity was observed in the pooled prevalence of anxiety (
index, significant heterogeneity was observed in the pooled prevalence of anxiety (  =99.6%, P=0.001), depression (
=99.6%, P=0.001), depression (  =99.4%, P=0.001), and insomnia (
=99.4%, P=0.001), and insomnia ( =99.6%, P=0.001).
=99.6%, P=0.001).
At the moment, many countries worldwide are facing the COVID-19 pandemic. Although limiting the crisis through a lockdown and widespread vaccination is important to reduce the virus's physical impacts, the pandemic's mental health consequences seem to be another substantial issue [3,4].
Health care workers (HCWs), who are directly involved in diagnosing, treating, and curing patients with COVID-19, are at risk for physical and mental problems. The HCWs are exposed to a heavy psychological burden due to the increasing number of suspected cases, overworking for long periods, lacking enough personal protective equipment, worrying about transmitting the disease to the family and friends, and lacking the required medications and sufficient support for all patients [5-8]. Since HCWs play a key role in controlling the epidemic and reducing the complications of the disease, maintaining their health is not only important from an individual point of view but also ensures the general public health. Previous studies have shown an increased prevalence of mental disorders among HCWs after initiating the Coronavirus pandemic. In a country-wide survey among HCWs conducted from March 2 to April 2, 2020, in China, the prevalence of depression and anxiety were 15.5% and 12.7%, respectively [9]. Moreover, the prevalence of depression and anxiety among HCWs during the COVID-19 pandemic was 28.1% and 33.1%, respectively, in a cross-sectional study in the UK [10].
At the beginning of this pandemic, all healthcare workers were under tremendous pressure. Excessive workload combined with fear of infection may cause mental disorders. The prevalence of mental disorders as an indicator of the imposed burden can show the importance of mental health in HCWs. On the other hand, the prevalence can vary over time with changes in factors such as better understanding of the disease and improvement in medical care facilities.
Differentiating short- and long-term impacts of the pandemic, in terms of time-horizon, on HCWs' mental health is necessary for policymaker guidance towards more evidence-based planning to overcome associated challenges. Thus, this systematic review and meta-analysis aimed to show the globally pooled prevalence of anxiety, depression, and insomnia among HCWs from a short-term perspective during the COVID-19 pandemic. To do so, individual studies conducted during the first 8 months after the onset of the pandemic were considered.
Materials and Methods
To conduct this systematic review and meta-analysis, PRISMA (Preferred Items for Reporting Systematic Reviews and Meta-Analyses) checklist was followed [11].
All relevant English articles on the prevalence of insomnia, anxiety, and depression among healthcare providers in dealing with COVID-19 were included in this review. Abstracts without full texts, editorials, case reports, and reviews were excluded from the study. Also, articles that did not use a valid questionnaire to measure anxiety, depression, and insomnia were excluded. Studies conducted on children, the general population, and hospitalized patients were excluded as well. Moreover, since the prevalence of an outcome in a case-control study cannot provide a good estimate in the reference population, such studies were also excluded.
To collect the data, two independent researchers searched databases of Web of Science, Scopus, Medline (PubMed), and Embase up to August 24, 2020. Moreover, preprint servers of medRxiv and SSRN were investigated. A search strategy was prepared using the combination of the following keywords: ("medical staff*" OR "Health Personnel" OR healthcare OR "Healthcare Worker*" OR "Health Care Provider*" OR "healthcare professional*") AND (COVID-19 OR "2019 novel coronavirus disease" OR "COVID-19 pandemic" OR "SARS-CoV-2 infection" OR "2019-nCoV infection" OR "coronavirus disease 2019" OR "severe acute respiratory syndrome coronavirus 2" OR 2019-nCoV OR "Wuhan coronavirus" OR SARS-CoV-2) AND (Depression OR "Depressive Symptom*" OR anxiety OR Nervousness OR insomnia OR "Sleep Initiation and Maintenance Disorders" OR "Early Awakening" OR "Sleep Initiation Dysfunction*" OR "mental health" OR psychological)
All identified studies were exported to the EndNote software (version X8, for Windows, Thomson Reuters, and Philadelphia, PA, USA). After removing the duplicates, two independent researchers evaluated titles and abstracts according to the study eligibility criteria. In the case of inconsistency between reviewers, a third reviewer assessed the eligibility criteria for the study to be included in the review.
Two independent researchers developed data extraction sheets to obtain relevant data, including the first author's name, publication date, occupation, study location, study design, sample size, response rate, age, and gender. The
prevalence of anxiety, depression, and insomnia, as well as outcome assessment methods and their cut-off points, were also collected. In the case of missing information, the necessary calculations were made.
The risk of bias in the primary studies was evaluated using the Newcastle-Ottawa quality assessment scale (NOS) for the case-control designs, and a customized version was developed for cross-sectional studies by two independent authors. The NOS is a star system developed to judge studies over three broad aspects: the selection of the study groups, the comparability of the groups, and the ascertainment of either exposure or outcome of interest. Each item on the scale is scored from one, which can be adapted to the specific topic of interest, to two. Thus, the maximum attainable stars (scores) for each study is nine, and studies with less than five stars indicate a high risk of bias [12].
In order to estimate the pooled prevalence of mental disorders among the medical staff during the COVID-19 pandemic within the 95% confidence interval (CI), the prevalence of anxiety, depression, and insomnia were examined in different articles from all over the world. Since CIs and standard errors (SEs) were not reported in some studies, the binomial distribution was applied to calculate them.
In the case of proportions near boundaries (in this instance, prevalence near 100% or zero), metan command was used to exclude the studies with such prevalence from the pooled estimate. Hence, the metaprop command was applied to estimate the exact binomial and score test based on CI for these proportions [13]. Also, the
 test at the 10% significant level (P<0.1) and the
test at the 10% significant level (P<0.1) and the  index were used to assess the between-study heterogeneity. According to the notable between-study heterogeneity, Der-Simonies and Laird random-effects models were used to calculate the pooled prevalence of anxiety, depression, and insomnia in medical staff [14].
index were used to assess the between-study heterogeneity. According to the notable between-study heterogeneity, Der-Simonies and Laird random-effects models were used to calculate the pooled prevalence of anxiety, depression, and insomnia in medical staff [14].Further, the pooled prevalence of anxiety, depression, and insomnia was estimated in different subgroups based on the variables such as gender, occupation, and the assessment tool. In order to reduce the strata of occupations, three categories of doctors, nurses, and other occupations (including administrative staff, technicians, public health administrators, midwives, residents, or medical students) were considered.
Moreover, a meta-regression analysis was carried out based on gender, occupation, and country of the study to investigate the potential source of heterogeneity. The publication bias was not examined in this study. Given that the estimated pooled prevalence and the probability of proportion are always positive numbers, any probable asymmetry in the funnel plot is not due to the publication bias [15]. In order to perform all statistical analyses, STATA 11 (StataCorp, College Station, TX, USA) was used.
Results
After the initial search through international databases, 1,907 studies were retrieved, the results of which were screened. Finally, 69 articles were included in the systematic review and meta-analysis. Fig.1 illustrates the process of selecting the relevant studies.
The total sample size for 69 included studies consisted of 102,349 medical staff. A total of 26,272 staff were male and 74,807 were female. According to occupation, 25,601 individuals were doctors, 47,449 were nurses, and 17,676 had other occupations within the medical realm. The evaluated studies (n = 69) were conducted in China (n = 31), Italy (n =7), Iran (n =3), and Turkey (n =3). Furthermore, two studies were conducted in each of the following countries: Oman, the USA, and Pakistan. In the following countries, one study was carried out: Thailand, Russia, Brazil, Switzerland, Korea, Taiwan, Philippines, Israel, Jordan, United Arab Emirates, Poland, Ecuador, Nepal, Saudi Arabia, Singapore, India, and Serbia. Moreover, one study was conducted in 30 countries, and one study was performed in two countries. Characteristics of the included studies are summarized in Table 1.
Risk of bias within studies: The NOS results for each study are presented in Supplementary Table 1.
Forest plots of pooled prevalence of mental health disorders (anxiety, depression, and insomnia) are presented in Figs. 2 to 4. Anxiety prevalence was estimated in 61 studies. In the present meta-analysis, the pooled prevalence of anxiety was 37% (95% CI: 31 to 43%). Depression was investigated in 50 studies. The pooled prevalence of depression was 34% (95% CI: 29 to 38%). Insomnia was estimated in 10 studies. The pooled prevalence of insomnia was 39% (95% CI: 25 to 53%) (Table 2).
According to the results of the
 test and
test and  index, significant heterogeneity was observed in the pooled prevalence of anxiety (
index, significant heterogeneity was observed in the pooled prevalence of anxiety (  =99.6%, P=0.001), depression (
=99.6%, P=0.001), depression (  =99.4%, P=0.001), and insomnia (
=99.4%, P=0.001), and insomnia ( =99.6%, P=0.001).
=99.6%, P=0.001).Table 1. Full description of the included articles published on anxiety, depression, and insomnia in healthcare workers
| First author (Publication Year) |
Country | Sample size (Response rate) |
Age* | Gender | Occupation | Outcome | |||||||||
| Male n (%) |
Female n (%) |
Doctor n (%) |
Nurse n (%) |
Other n (%) |
Anxiety | Depression | Insomnia | ||||||||
| Assessment cut-off |
n (%) |
Assessment cut-off |
n (%) |
Assessment cut-off |
n (%) |
||||||||||
| Ahmed, M. A. (2020)[16] | Worldwide (30 countries) |
650 (97.1) |
NR | 160 (24.6) |
490 (75.3) |
0 |
0 | 650 (100) |
NR | 585 (90) |
- | - | - | - | |
| Alshekaili,M. (2020)[17] | Oman | 1,139 (97.6) |
36.3 ± 6.5 | 228 (20.0) | 911 (80.0) | 384 (33.7) | 449 (39.5) | 305 (26.8) | DASS-21 ≥8 |
388 (34.1) |
DASS-21 ≥10 |
368 (32.3) |
ISI ≥14 |
211 (18.5) |
|
| Amerio, A. (2020)[18] | Italy | 131 (25) |
52.3 ± 12.2 | 68 (51.9) |
63 (48.0) |
131 (100) |
0 | 0 | - | - | PHQ-9 ≥10 |
30 (22.9) |
- | - | |
| An, Y. (2020)[19] | China | 1,103 NR |
32.2 ± 7.6 | 102 (9.2) |
1,001 (90.7) |
0 | 1,103 (100) |
0 | - | - | PHQ-9 ≥5 |
481 (43.6) |
- | - | |
| Apisarnthanarak, A. (2020)[20] | Thailand | 160 NR |
32 (23–62range) | 65 (40.6) |
95 (59.4) |
52 (32.5) |
61 (38.1) |
47 (29.4) |
GAD-7 ≥5 |
68 (42.5) |
- | - | - | - | |
| Bachilo, E. (2020)[21] | Russia | 812 (100) |
NR | 154 (19) |
658 (81) |
641 (79.0) |
146 (17.9) |
25 (3.1) |
GAD-7 ≥5 |
396 (48.7) |
PHQ-9 ≥5 |
468 (57.6) |
- | - | |
| Badahdah, A. (2020)[22] | Oman | 509 NR |
37.6 ± 7.6 | 100 (19.7) |
407 (80.3) |
194 (38.1) | 315 (61.9) | 0 | GAD-7 ≥5 |
328 (64.5) |
- | - | - | - | |
| Barello, S. (2020)[23] | Italy | 376 (32.6) |
40 ± 11 | 99 (26.3) |
277 (73.6) |
67 (17.8) | 271 (72.1) | 38 (10.1) | - | - | MBI ≥4 |
195 (51.8) |
- | - | |
| Buselli, R. (2020)[24] | Italy | 106 (41) |
50 ± 9.9 | 27 (25.5) |
79 (74.5) |
0 | 58 (55) |
48 (45) |
STAI ≥40 |
57 (54) |
- | - | - | - | |
| Cai, H. (2020)[25] | China | 534 NR |
36.4 ± 16.1 | 167 (31.3) |
367 (68.7) |
233 (43.6) | 248 (46.4) | 53 (9.9) | NR | 436 (81.6) |
- | - | - | - | |
| Çalişkan, F. (2020)[26] | Turkey | 290 NR |
31.8 ± 6.9 | 179 (61.7) |
111 (38.2) |
290 (100) |
0 | 0 | HADS ≥10 |
103 (35.5) |
HADS >7 |
180 (62) |
- | - | |
| Cao, J. (2020)[27] | China | 102 (97.10) |
31.7 ± 6.8 | 25 (24.5) |
77 (75.5) |
40 (39.2) | 54 (52.9) | 8 (7.8) |
- | - | PHQ-9 >10 |
7 (6.9) |
- | - | |
| Chatterjee, S. S. (2020)[28] | India | 152 NR |
42.0 ± 12.2 | 119 (78.3) |
33 (21.7) |
152 (100) |
0 | 0 | DASS-21 NR |
60 (39.5) |
DASS-21 NR |
53 (34.9) |
- | - | |
| Chen, J. (2020)[29] | China | 900 NR |
36.4 ± 8.5 | 281 (31.2) |
619 (68.3) |
541 (60.1) |
311 (34.5) |
48 (5.3) |
GAD-7 ≥10 |
150 (16.7) |
PHQ-9 ≥10 |
164 (18.3) |
- | - | |
| Chen, X. (2020)[30] | Ecuador | 252 (62.8) |
NR | 87 (34.5) |
165 (65.5) | NR | NR | NR | GAD-7 ≥10 |
71 (28.2) |
- | - | - | - | |
| Cheng, F. F. (2020)[31] | China | 534 NR |
NR | 94 (17.6) |
440 (82.4) |
289 (54.1) |
245 (45.9) |
0 | SAS ≥50 |
75 (14.0) |
- | - | PSQI >7 |
160 (30.0) |
|
| Chew, N. W. S. (2020)[32] | Singapore and India |
906 (90.6) |
29(25-35)£ | 323 (35.7) | 583 (64.3) | 268 (29.6) | 355 (39.2) | 283 (31.2) |
DASS-21 >7 |
142 (15.7) | DASS-21 >9 |
96 (10.6) | - | 190 (21.0) |
|
| Civantos, A. M. (2020)[33] | USA | 349 (7.8) |
NR | 212 (60.7) | 137 (39.3) | 349 (100) |
0 | 0 | GAD-7 ≥5 |
167 (47.9) | PHQ-2 ≥3 |
37 (10.7) |
- | - | |
| Consolo, U. (2020)[34] | Italy | 356 (40.7) |
NR | 215 (60.4) | 141 (39.6) |
356 (100) |
0 | 0 | GAD-7 ≥5 |
204 (57.3) |
- | - | - | - | |
| Croll, L. (2020)[35] | USA | 130 (51) |
NR | NR | NR | NR | NR | NR | NR | 108 (83) | NR | 49 (38) |
- | - | |
| Dal'Bosco, E. B.(2020)[36] | Brazil | 88 (18.5) |
NR | 9 (10.2) |
79 (89.8) |
0 | 88 (100) |
0 | HADS >7 |
43 (48.9) | HADS >8 |
22 (25) | - | - | |
| Dong, Z. Q. (2020)[37] | China | 4,618 NR |
NR | 755 (16.3) | 3,863 (86.7) | 1,138 (24.6) | 2,889 (62.6) | 591 (12.8) | HEI ≥8 |
24.2% anxiety or/and depressive symptoms | - | - | |||
| Elbay, R. Y. (2020)[38] | Turkey | 442 NR |
36.0 ±8.7 | 191 (43.2) | 251 (56.8) | 442 (100) |
0 | 0 | DASS-21 NR |
224 (51.6) |
DASS-21 NR |
286 (64.7) |
- | - | |
| Giusti, E. M. (2020)[39] | Italy | 330 (41.2) |
44.6 ± 13.5 | 124 (37.4) | 206 (62.6) | 140 (42.2) | 86 (26.1) | 105 (31.8) |
DASS-21 >75th percentile |
103 (31.3) | DASS-21 >75th percentile |
88 (26.8) | - | - | |
| Guo, J. (2020)[40] | China | 11,118 NR |
NR | 2,802 (25·2) | 8,316 (74.8) |
3,351 (30·1) | 5,900 (53·1) | 1,671 (15.0) |
SAS ≥50 |
1,940 (17.4) |
SDS ≥50 |
3,497 (31.4) |
- | - | |
| Hassannia, L. (2020)[41] | Iran | 487 NR |
NR | NR | NR | 127 (6.2) | 105 (5.10) | 255 (52.4) |
HADS >11 |
167 (34.3) |
HADS >11 |
121 (24.8) |
- | - | |
| He, J. (2020)[42] | China | 4,403 NR |
NR | 1,092 (24.8) |
3,311 (75.2) |
905 (20.5) | 746 (16.9) | 2,752 (62.5) |
SAS ≥50 |
980 (22.3) |
SDS ≥52 |
1,222 (27.7) |
- | - | |
| Hu, D. (2020)[43] | China | 2,014 (99.6) |
30.9±6.1 | 260 (12.9) | 1,754 (87.1) | 0 | 2,014 (100) |
0 | SAS ≥50 |
833 (41.3) |
SDS ≥53 |
878 (43.6) |
- | - | |
| Huang, L. (2020)[44] | China | 364 (96.6) |
32 (27–40)£ | 150 (41) |
214 (59) |
0 | 119 (32.7) | 245 (67.3) | SAS ≥50 |
85 (23.3) |
- | - | - | - | |
| Kaveh, M. (2020)[45] | Iran | 1,038 NR |
36.3±8.2 | 129 (12.4) | 909 (87.6) | 214 (20.6) | 514 ( 49.5) |
310 (29.9) |
BAI ≥8 |
1,038 (100) |
- | - | - | - | |
| Labrague, L. (2020)[46] | Philippines | 325 (93) |
30.9±6.6 | 82 (25.2) |
243 (74.8) | 0 | 325 (100) |
0 | CDAS ≥9 |
123 (37.8) |
- | - | - | - | |
| Lai, J. (2020)[6] | China | 1,257 (68.7) |
NR | 293 (23.3) | 964 (76.7) | 493 (39.2) | 764 (60.8) | 0 | GAD-7 ≥5 |
560 (44.6) |
PHQ-9 ≥5 |
634 (50.4) |
ISI ≥8 |
427 (34.0) |
|
| Lin, Z. (2020)[47] | China | 636 (25) |
33·5 ± 8·5 | 99 (52·1) | 91 (47·9) | 190 (29·9) | 297 (46·7) | 149 (23·4) | DASS-21 ≥7 |
161 (25·3) | - | - | - | - | |
| Liu, C. Y. (2020)[48] | China | 512 (85.3) |
NR | 79 (15.4) |
433 (84.5) | NR | NR | NR | SAS ≥50 |
64 (12.5) |
- | - | - | - | |
| Liu, S. (2020)[49] | China | 6,588 (94.0) |
NR | 2,212 (33.5) |
4,370 (66.4) |
2,523 (38.3) |
3,888 (59.0) |
177 (2.7) |
- | - | PHQ-9 ≥10 |
3,795 (57.6) |
- | - | |
| Liu, Z. (2020)[50] | China | 4,679 (100) |
35.9 ± 9 | 830 (17.7) |
3,849 (82.3) |
1,853 (39.6) | 2,826 (60.4) | 0 | SAS ≥50 |
749 (16.0) |
SDS ≥50 |
1,619 (34.6) |
- | - | |
| Lu, W. (2020)[51] | China | 2,299 (94.8) |
NR | 514 (22.4) |
1,785 (77.6) |
2,042 (88.8) |
0 | 257 (11.2) |
HAMA ≥7 |
569 (24.7) |
HAMD ≥7 |
268 (11.6) |
- | - | |
| Ma, Y. (2020)[52] | China | 34 (100) |
NR | 10 (29.4) |
24 (71) |
20 (59) |
14 (41) |
0 | GAD-7 ≥5 |
12 (35) | PHQ-9 ≥5 |
8 (24) |
- | - | |
| Magnavita, N. (2020)[53] | Italy | 595 (82) |
NR | 175 (29.9) | 417 (70.1) | NR | NR | NR | GADS ≥5 |
99 (16.6) | GADS ≥2 |
121 (20.3) | - | - | |
| Mahendran, K. (2020)[54] | China | 120 (96) |
35 (19–63)£ | 28 (23) |
87 (73) |
14 (12) |
60 (50) |
46 (38.3) |
GAD-7 NR |
64 (53.3) |
- | - | - | - | |
| Naser, A. Y. (2020)[55] | Jordan | 1,163 NR |
NR | 510 (43.8) |
653 (56.2) | 560 (48.2) |
151 (13) |
452 (38.8) |
GAD-7 ≥5 |
823 (70.7) |
PHQ-9 ≥5 |
907 (77.9) |
- | - | |
| Qi, J. (2020)[56] | China | 1,306 (93.6) |
33.1 ± 8.4 |
256 (19.6) | 1,050 (80.4) | NR | NR | NR | - | - | - | - | PSQI >6 AIS>6 |
936 (71.7) 594 (45.5) |
|
| Que, J. (2020)[57] | China | 2,285 (78) |
31.1 ± 6.99 | 707 (30.9) | 1,578 (69.1) | 860 (37.6) | 208 (9.1) | 1,217 (53.2) |
GAD-7 ≥5 |
1,233 (53.9) | PHQ-9 ≥5 |
1,271 (55.6) | ISI ≥8 |
1,628 (71.2) | |
| Rossi, R. (2020)[58] | Italy | 1,379 NR |
39.0 ± 16.0 | 315 (22.8) |
1,064 (77.2) |
519 (37.4) |
472 (34.2) |
387 (28.1) |
GAD-7 ≥15 |
273 (19.8) | PHQ-9 ≥15 |
341 (24.7) | ISI ≥22 |
114 (8.2) | |
| Saddik, B. (2020)[59] | United Arab Emirates |
1,385 (93.3) |
20.5 ± 2.3 | 391 (28.2) | 994 (71.8) | 0 | 0 | 1,385 (100) | GAD-7 ≥5 |
520 (37.5) |
- |
- |
- |
- |
|
| Salman, M. (2020)[60] | Pakistan | 398 NR |
28.6 ± 4.1 | 183 (46.0) | 215 (54.0) | 205 (51.5) | 133 (33.4) | 60 (15.1) | GAD-7 ≥10 |
85 (21.3) |
PHQ-9 ≥5 |
255 (64.1) |
- | - | |
| Sandesh, R. (2020)[61] | Pakistan | 112 (100) |
NR | 64 (57.1) |
48 (42.9) |
NR | NR | NR | DASS-21 NR |
107 (95.5) |
DASS-21 NR |
101 (90.2) |
- | - | |
| Savitsky, B. (2020)[62] |
Israel | 215 (88) |
NR | NR | NR | 0 | 0 | 215 (100) |
GAD-7 ≥10 |
92 (42.8) |
- | - | - | - | |
| Sögüt, S. (2020)[63] | Turkey | 972 NR |
20.8 ± 1.9 | 0 | 972 (100) |
0 | 0 | 972 (100) |
BAI ≥22 |
54 (5.5) |
- | - | - | - | |
| Song, X. (2020)[64] | China | 14,825 (100) |
34.0 ± 8.2 | 5,289 (35.7) | 9,536 (64.3) |
6,093 (41.1) |
8,732 (58.9) |
0 | - | - | CES-D ≥16 |
3,733 (25.2) | - | - | |
| Stojanov, J. (2020)[65] | Serbia | 83 (70) |
39.1 ± 7.3 | 36 (43.37) |
47 (56.6) |
NR | NR | NR | GAD-7 ≥10 |
27 (31.8) |
SDS ≥60 |
15 (17.6) |
- | - | |
| Sung, C. (2020)[66] | Taiwan | 1,795 NR |
36.7 ± 8.2 | 360 (20.1) |
1,435 (79.9) | 357 (19.9) |
1,064 (59.3) | 374 (20.8) |
STAI-6 ≥37 |
1,610 (89.7) |
CES-D-10 ≥10 |
817 (45.5) |
- | - | |
| Szepietowski, J. C. (2020)[67] | Poland | 120 (97.6) |
44.4 ± 11.9 | 26 (21.7) |
94 (78.3) |
58 (48.3) | 62 (51.7) | 0 | GAD-7 ≥5 HADS-A ≥8 |
54 (45.0) 35 (29.1) |
PHQ-9 ≥10 HADS-D ≥8 |
24 (20) 17 (14.1) |
- |
- |
|
| Tan, B. Y. Q. (2020)[68] | Singapore | 470 (94) |
30 (28–35)£ | 149 (31.7) | 321 (68.3) | 135 (28.7) | 161 (34.3) | 174 (37.0) |
DASS-21 A>7 |
68 (14.5) |
DASS-21 D>9 |
42 (8.9) |
- | - | |
| Temsah, M. H. (2020)[69] | Saudi Arabia | 582 (71.8) |
NR | 145 (24.91) |
437 (75.1) |
NR | 363 (62.4) |
NR | GAD-7 (≥5) |
185 (31.8) |
- | - | - | - | |
| Teng, Z. (2020)[70] | China | 398 NR |
NR | 96 (24.1) |
302 (75.9) |
NR | NR | NR | SAS ≥50 |
56 (14.1) |
PHQ-9 ≥5 |
143 (35.9) |
- | - | |
| Thapa, L. (2020)[71] | Nepal | 100 NR |
26.8 ± 8.17 | 22 (22.0) |
78 (78.0) |
9 (9.0) |
62 (62.0) |
29 (29.0) |
ALI≥1 SAS≥45 |
98(98) 34 34) |
- |
- |
- |
- |
|
| Vafaei, H. (2020)[72] | Iran |
575 (95.9) |
NR | 0 | 599 (100) |
194 (32.4) | 275 (45.9) | 130 (21.7) | - | - | PHQ-9 ≥5 |
383 (66.6) |
- | - | |
| Wang, H. (2020)[73] | China | 1,045 (80.1) |
NR | 148 (14.2) | 897 (85.8) | 149 (14.3) | 773 (74.0) | 123 (11.7) | HADS-A ≥8 |
499 (47.8) | HADS-D ≥8 |
412 (39.4) | ISI ≥8 |
521 (49.9) |
|
| Weilenmann, S. (2020)[74] | Switzerland | 1,410 NR |
34 (29-46)£ | 476 (33.7) |
934 (66.2) |
857 (60.8) | 553 (39.2) | 0 | GAD-7 ≥10 |
365 (25.9) |
PHQ-9 ≥10 |
292 (20.7) | - | - | |
| Xiao, H. (2020)[75] | China | 933 (87.9) |
NR | 279 (29.9) | 654 (70.1) | NR | NR | 933 (100) |
GAD-7 ≥5 |
160 (17.1) |
PHQ-9 ≥5 |
236 (25.3) |
- | - | |
| Xiao, X. (2020)[76] | China | 958 NR |
NR | 314 (32.8) |
644 (67.2) |
378 (39.5) |
359 (37.5) |
221 (23.0) |
HADS ≥8 |
518 (54.1) |
HADS ≥8 |
549 (57.3) |
- | - | |
| Xiaoming, X. (2020)[77] | China | 8817 NR |
33.2 ± 8.2 | 1943 (22.0) | 6874 (78.0) | 3212 (36.4) | 4685 (53.1) | 920 (10.4) | GAD-7 ≥5 |
1825 (20.7) |
PHQ-9 ≥5 |
2666 (30.2) |
- | - | |
| Xing, J. (2020)[78] | China | 548 (97.9) |
NR | 153 (27.9) | 395 (72.1) | 137 (25.00) | 411 (75.00) | 0 | SCL-90 NR |
187 (34.1) |
SCL-90 NR |
163 (29.7) |
- | - | |
| Yang, S. (2020)[79] | Korea | 65 (89.0) |
NR | 34 (52.3) |
31 (47.7) |
65 (100) |
0 | 0 | GAD-7 ≥5 |
21 (32.3) | PHQ-9 ≥10 |
12 (18.5) |
- | - | |
| Zhang, C. (2020)[80] | China | 1,563 NR |
NR | 270 (17.2) | 1,293 (82.7) | 454 (29.0) |
984 (62.9) |
125 (8.0) |
GAD-7 ≥5 |
76 (44.7) |
PHQ-9 ≥5 |
488 (50.7) |
ISI ≥8 |
564 (36.1) |
|
| Zhang, W. R. (2020)[81] | China | 2,182 NR |
NR | 781 (35.8) |
1,401 (64.2) |
680 (31.2) |
247 (11.3) |
1255 (57.5) |
GAD-2 ≥3 |
228 (10.4) |
PHQ-2 ≥3 |
232 (10.6) |
ISI >8 |
739 (33.9) |
|
| Zhu, J. (2020)[82] | China | 165 (100) |
34.1 ± 8.0 | 28 (17) |
137 (83) |
79 (47.9) |
86 (52.1) |
0 | SAS >50 |
33 (20.0) |
SDS >50 |
73 (42.2) |
- | - | |
| Zhu, Z. (2020)[83] | China | 5,062 (77.1) |
NR | 758 (15) |
4,304 (85.0) |
1,004 (19.8) |
3,417 (67.5) |
641 (12.7) |
GAD-7 ≥8 |
1,218 (24.1) |
PHQ-9 ≥10 |
681 (13.5) |
- | - | |
*(mean ± standard deviation, year). All studies are cross-sectional. £ Median age (IQR). NR: Not report.
DASS-21: Depression, Anxiety, and Stress Scale-21 Items. PHQ-9: 9-item Patient Health Questionnaire. GAD-7: Generalized Anxiety Disorder 7‐ Item scale. MBI: Maslach Burnout Inventory. STAI: State-Trait Anxiety Inventory. BAI: Beck Anxiety Inventory. ISI: Insomnia Severity Index. HADS: Hospital Anxiety and Depression Scale. SAS: Self-Rating Anxiety Scale. HAMA: Hamilton Anxiety Scale. HAMD: Hamilton Depression Scale. CES-D: Center for the Epidemiological Studies of Depression. ALI: Anxiety Level Index. HEI: Huaxi Emotional-Distress Index. CDAS: COVID-19 Anxiety Scale. STAI: State-Trait Anxiety Inventory. PSQI: Pittsburgh Sleep Quality Index. AIS: Athens Insomnia Scale. SAS: Self-Rated Anxiety Scale.
DASS-21: Depression, Anxiety, and Stress Scale-21 Items. PHQ-9: 9-item Patient Health Questionnaire. GAD-7: Generalized Anxiety Disorder 7‐ Item scale. MBI: Maslach Burnout Inventory. STAI: State-Trait Anxiety Inventory. BAI: Beck Anxiety Inventory. ISI: Insomnia Severity Index. HADS: Hospital Anxiety and Depression Scale. SAS: Self-Rating Anxiety Scale. HAMA: Hamilton Anxiety Scale. HAMD: Hamilton Depression Scale. CES-D: Center for the Epidemiological Studies of Depression. ALI: Anxiety Level Index. HEI: Huaxi Emotional-Distress Index. CDAS: COVID-19 Anxiety Scale. STAI: State-Trait Anxiety Inventory. PSQI: Pittsburgh Sleep Quality Index. AIS: Athens Insomnia Scale. SAS: Self-Rated Anxiety Scale.
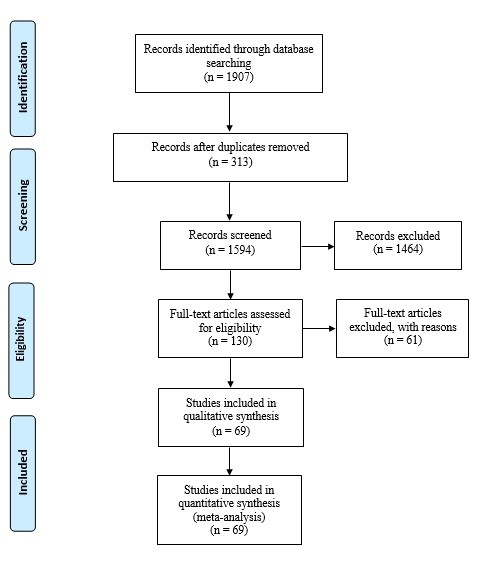
Fig. 1. PRISMA flowchart of different phases in searching the relevant publications

Fig. 2. Forest plot of pooled prevalence of anxiety in healthcare workers
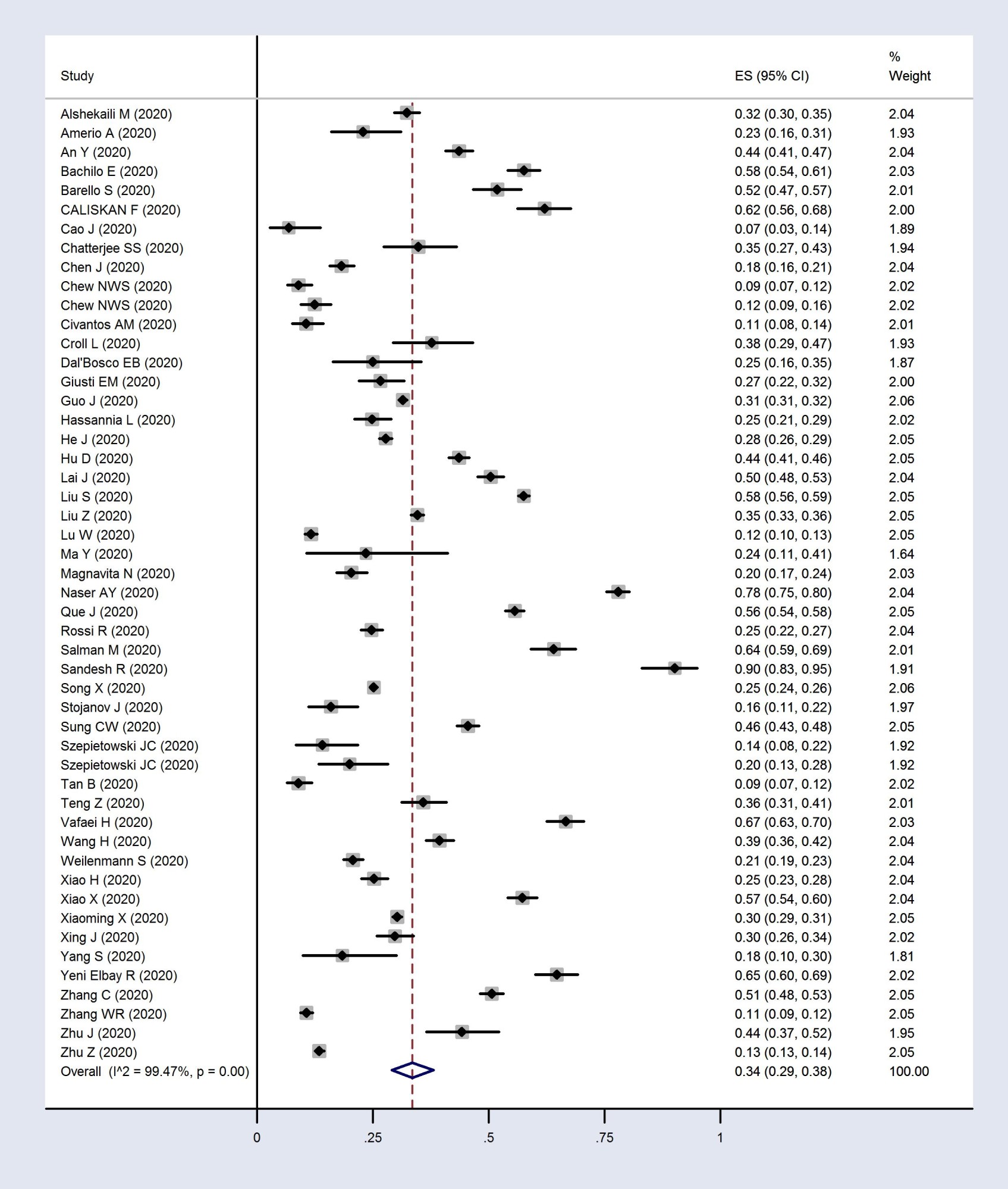
Fig. 3. Forest plot of pooled prevalence of depression in healthcare workers

Fig. 4. Forest plot of pooled prevalence of insomnia in healthcare workers
The results of the subgroup analysis are presented in Table 2. The pooled prevalence of anxiety in male and female subgroups was 36% (95%CI: 23 to 50%) and 39% (95%CI: 30 to 49%), respectively. In addition, the pooled prevalence of anxiety by occupation type was 37% (95%CI: 27 to 47%) among doctors, 42% (95%CI: 34 to 50%) among nurses, and 35% (95%CI: 21 to 50%) in other groups. Also, a subgroup analysis was conducted according to the assessment tool; accordingly, the pooled prevalence of anxiety by scales such as BAI, DASS-21, GAD-7, HADS, SAS, and STAI were 63% (95%CI: 61 to 65%), 35% (95%CI: 24 to 48%), 33% (95%CI: 28 to 46%), 42% (95%CI: 34 to 50%), 21% (95%CI: 16 to 26%), and 88% (95%CI: 87 to 90%), respectively.
The pooled prevalence of depression in male and female subgroups was 32% (95%CI: 20 to 45%) and 36% (95%CI: 25 to 48%), respectively. The pooled prevalence of depression was 30% (95%CI: 20 to 42%) in doctors, 33% (95%CI: 24 to 42%) in nurse, and 27% (95%CI: 12 to 45%) in other groups. The pooled prevalence of depression by the assessment tool was 27% (95%CI: 27 to 28%), 33% (95%CI: 18 to 51%), 37% (95%CI: 24 to 50%), 37% (95%CI: 27 to 44%), 11% (95%CI: 9 to 12%), and 36% (95%CI: 31 to 41%) in subgroups of CES-D, DASS-21, HADS, PHQ-9, PHQ-2, and SDS, respectively.
The pooled prevalence of depression in male and female subgroups was 32% (95%CI: 20 to 45%) and 36% (95%CI: 25 to 48%), respectively. The pooled prevalence of depression was 30% (95%CI: 20 to 42%) in doctors, 33% (95%CI: 24 to 42%) in nurse, and 27% (95%CI: 12 to 45%) in other groups. The pooled prevalence of depression by the assessment tool was 27% (95%CI: 27 to 28%), 33% (95%CI: 18 to 51%), 37% (95%CI: 24 to 50%), 37% (95%CI: 27 to 44%), 11% (95%CI: 9 to 12%), and 36% (95%CI: 31 to 41%) in subgroups of CES-D, DASS-21, HADS, PHQ-9, PHQ-2, and SDS, respectively.
Table 2. The pooled prevalence of mental health disorders in various subgroups
| No. of studies | Prevalence of anxiety (%) (95%CI) |
No. of studies | Prevalence of depression (%) (95%CI) |
No. of studies | Prevalence of insomnia (%) (95%CI) |
||
| Total | 60 | 37 (31-43) | 48 | 34 (29-38) | 9 | 39 (25-53) | |
| Gender | Male | 11 | 30 (23-50) | 10 | 32 (20-45) | 3 | 22 (12-34) |
| Female | 12 | 39 (30-49) | 12 | 36 (25-48) | 3 | 27 (11-46) | |
| Occupation | Doctor | 16 | 37 (27-47) | 14 | 30 (20-42) | 3 | 34 (6-71) |
| Nurse | 16 | 42 (34-50) | 13 | 33 (24-42) | 3 | 37 (11-68) | |
| Other medical staff | 11 | 35 (21-50) | 6 | 27 (12-45) | 3 | 34 (6-71) | |
| Assessment Scale | BAI | 2 | 63 (61-65) | - | - | - | - |
| GAD-7 | 25 | 33 (26-40) | - | - | - | - | |
| SAS | 10 | 21 (16-26) | - | - | - | - | |
| STAI-6 | 2 | 88 (87-90) | - | - | - | - | |
| DASS-21 | 9 | 35 (24-48) | 8 | 33 (18-51) | - | - | |
| HADS | 6 | 42 (34-50) | 6 | 37 (24-50) | - | - | |
| CES-D | - | - | 2 | 27 (27-28) | - | - | |
| PHQ-9 | - | - | 21 | 37 (28-46) | - | - | |
| PHQ-2 | - | - | 2 | 11 (9-12) | - | - | |
| SDS | - | - | 5 | 36 (31-40) | - | - | |
| ISI | - | - | - | - | 6 | 29 (0.18-0.41) | |
| PSQI | - | - | - | - | 2 | 60 (0.58-0.62) |
The pooled prevalence of insomnia in medical staff was 22% (95%CI: 12 to 34%) and 27% (95%CI: 11 to 46%) among males and females, respectively. Furthermore, the pooled prevalence of insomnia according to the assessment tools of ISI and PSQI was 29% (95%CI: 18 to 41%) and 60% (95%CI: 58 to 62%), respectively.
According to the univariate and multivariate meta-
regression analysis, as given in Table 3, only the country of the study had a significant association with the prevalence of anxiety (P<0.05). One reason for the high heterogeneity in this study was the different prevalence reported in each country. However, there was no significant association for other variables (P>0.05).
According to the univariate and multivariate meta-
regression analysis, as given in Table 3, only the country of the study had a significant association with the prevalence of anxiety (P<0.05). One reason for the high heterogeneity in this study was the different prevalence reported in each country. However, there was no significant association for other variables (P>0.05).
Table 3. Meta-regression analysis for the effect of the suspected variables on the pooled prevalence of anxiety, depression, insomnia in medical staff
| Pooled prevalence | Variable | Univariate model | Multivariable model | ||||
| β | SE | P-Value | β | SE | P-Value | ||
Anxiety |
Gender | 1.08 | 3.01 | 0.72 | 0.78 | 2.9 | 0.7 |
| Occupation | -1.1 | 4.3 | 0.79 | -1.5 | 4.3 | 0.7 | |
| Country | 9.9 | 3.8 | 0.01 | 9.9 | 3.8 | 0.01 | |
Depression |
Gender | 0.34 | 2.7 | 0.9 | -0.02 | 2.8 | 0.9 |
| Occupation | -1.5 | 4.1 | 0.7 | -1.4 | 4.2 | 0.7 | |
| Country | -3.02 | 3.8 | 0.4 | -2.9 | 3.9 | 0.4 | |
Insomnia |
Gender | 11.1 | 7.6 | 0.1 | 12.3 | 7.5 | 0.1 |
| Occupation | -1.01 | 11.5 | 0.3 | -3.4 | 11.2 | 0.7 | |
| Country | -27.1 | 16.1 | 0.1 | -29.6 | 16.1 | 0.08 | |
SE: standard error, β: regression coefficient
Discussion
This systematic review and meta-analysis showed a high prevalence of psychiatric disorders among healthcare personnel during the COVID-19 crisis. Based on its results, the pooled prevalence rates of anxiety, depression, and insomnia were 37%, 34%, and 39%, respectively.
The findings showed that a high proportion of HCWs experienced considerable mental health disorders during the COVID-19 pandemic. This work, similar to many previous ones, implies the importance and urgency of attention to the mental health of medical staff.
Compared with the original systematic review (87), a higher prevalence of mental disorders was found (23.21% vs. 37% for anxiety, 22.8% vs. 34% for depression, 34.32% vs. 39% for insomnia in the original and present review, respectively). The pandemic of the new coronavirus is associated with many potential stressors that can lead to psychological problems and adverse consequences, especially among medical staff directly dealing with the crisis. Therefore, a high burden of mental health disorders is expected among them. In addition, the current review includes studies conducted over a longer period from the beginning of the epidemic. The fact that some countries have failed to control the disease despite many efforts and the number of disease cases is increasing worldwide may have caused more anxiety and fear among the medical staff.
Anxiety related to COVID-19: Anxiety disorders are defined as excess worries and fears that debilitate and cause a loss of quality of life [84, 85]. The present review findings showed that a large number of HCWs felt anxious about the prevalence of the COVID-19 pandemic. Anxiety in healthcare providers during the COVID-19 pandemic can be caused by factors such as shortage of PPE, fear of contact with infected people, getting infected and spreading the disease to families and friends, and fear of death [86, 87]. Healthcare professionals might be at a higher risk for developing anxiety disorder because of the emerging and life-threatening nature of the new coronavirus, increased workload and fatigue, lack of self-efficacy, and insufficiency of social support [88]. In this regard, social and economic consequences can result in more concerns [86]. In a survey conducted in Wuhan City in China, 63.2% and 28.0% of the frontline nurses reported moderate and severe levels of fear, respectively. Additionally, 11.0% and 3.3% of these nurses had moderate and severe anxiety levels [88].
In this review, the prevalence of anxiety was higher in female HCWs than in males (39% vs. 30%). In the same line, a previous study indicated that the Self-Rating Anxiety Scale for female nurses was higher than for males, indicating a higher level of anxiety among females [88]. A previous systematic review and meta-analysis among HCWs showed anxiety disorder to be more prevalent in females than males (29.06% vs. 20.92%, respectively) [89]. Nurses working in different units also noted that anxiety was more likely among women than men [90, 91]. Sex differences in the occurrence of anxiety can be due to genetic, neurodevelopmental, environmental, and neurobiological factors. Brain structural and functional differences, as well as hormonal differences between men and women, may have a critical role in the neurobiology of anxiety disorders. There are differences between the brain of men and women in areas dependent on anxiety, including the prefrontal cortex, hippocampus, and extended amygdala complex. Moreover, estrogen and progesterone, as female reproductive hormones, can play a key role in the neurobiology of anxiety disorder. Periodic fluctuations in these hormones throughout a woman's life can also precipitate Hypothalamic-Pituitary-Adrenal axis responses. These large fluctuations in sex hormone levels may contribute to changes in the severity of anxiety symptoms at different stages of reproduction in women [91]. Thus, female medical staff are assumed to be a more vulnerable group affected more severally by anxiety; accordingly, this disorder may be a much more important issue in women.
Depressive disorders: Depression is characterized by slow psychic processes, depressed and/or irritable mood, reduced energy, sad feelings, disinterest, apathy or psychomotor agitation, difficulty in concentrating, negative thoughts, loss of planning capacity, and altered judgment of the situation [36].
During the COVID-19 pandemic, a high frequency of depressive cases was reported among HCWs worldwide. For example, in a systematic review of 59 studies, the prevalence of depression was reported within the range of 5% to 51% [92]. In another systematic review and meta-analysis, the pooled prevalence of depression was 36% among the health professionals, based on a random-effects model (95%CI: 0.19 to 0.58) [93].
Furthermore, witnessing the suffering of patients with COVID-19 and being incapable of saving the lives of some patients make the medical staff upset. In the long run, this issue can make HCWs prone to depression and other psychological diseases since depression is often comorbid with anxiety [94]. Consequently, causative factors of anxiety in HCWs, such as insufficient understanding of the disease, lack of prevention knowledge, fear of getting infected, and transmission of the infection to family members, predispose the staff to depression.
In a survey in China, the researchers found that insufficient PPE and a history of contact with diagnosed COVID-19 patients were two independent risk factors for developing depression among HCWs. In this regard, having no contact with the COVID-19 patients was found as a protective factor [76]. In a cross-sectional survey in China, gender (male) was considered a protective factor for depression among doctors [82]. This finding was consistent with the present review results; the prevalence of depression in female HCWs was higher than the males (36% vs. 32%).
Given the confirmed findings that depression is generally more common in females [95, 96], authorities are required to take measures to prevent and control depression in female HCWs.
Insomnia related to COVID-19: Insomnia disorder refers to the difficulty in falling or staying asleep, poor sleep quality, or less sleep duration. This disorder often co-occurs with other mental illnesses, such as depression. Insomnia also may lead to physical and mental morbidities and reduce the quality of life [97].
In the critical situation caused by the COVID-19 outbreak, HCWs experience different levels of insomnia [92, 98]. In the present review, a high prevalence of insomnia was reported among the medical staff. This disorder was especially more common among nurses and women. These findings were in line with a previous systematic review and meta-analysis indicating that the pooled prevalence of sleep disturbances was significantly lower among male HCWs than the females (33.8% vs. 46.4% p < 0.001). Additionally, the prevalence of sleep disturbances among nurses was higher than among doctors [99].
In general, gonadal steroid effects are a potential reason for the increased prevalence of insomnia among females compared with males [100]. Considering the direct association of depression with insomnia and the high prevalence of depression among women in this study, a high frequency of insomnia is also expected.
Nurses responsible for taking care of patients with COVID-19 are at a higher risk of infection because they are in close and frequent contact with such patients and should work longer hours than usual [6]. Consequently, such a situation may play a role in causing insomnia. Furthermore, anxiety, depression, and insomnia are closely related to their risk factors. In a study carried out among the medical health workers in China, the history of organic diseases, residence in rural areas, risk of contact with COVID-19 patients, and female gender were among the independent risk factors for insomnia, anxiety, and depression [81]. Shift working, increased workload, education level, and worrying about getting infection were also among the other risk factors for developing insomnia [98, 101].
The strength of this systematic review is that it includes a wide range of published articles covering a large sample size. In the case of the study limitations, the following issues can be mentioned: an inherent and considerable heterogeneity was observed in the pooled prevalence of anxiety, depression, and insomnia. Hence, a random-effects model was applied to calculate the pooled prevalence of outcomes. Subsequently, subgroup analysis and a meta-regression model were conducted. Moreover, since the included articles used different tools to measure the participants' mental health disorders, the pooled prevalence of outcomes may be questionable. In this vein, a subgroup analysis was conducted based on the assessment tools. Another limitation of this review was the low quality of some included studies.
To the best of the authors' knowledge, this study is the most comprehensive systematic review and meta-analysis of primary studies on the prevalence of anxiety, depression, and insomnia in HCWs during the Coronavirus pandemic. However, one of the limitations of this study was the unavailability of the full text of some articles, ultimately leading to the exclusion of such articles from the meta-analysis. In addition, the low quality of some included articles was another limitation.
Conclusion
The findings indicate a high impact of the COVID-19 pandemic on the mental health of HCWs involved in the crisis in various territories and occupations among both genders. The medical staff's mental health is as crucial as their physical health. Moreover, mental health is important not only for the medical professionals' well-being but also for their work efficacy, improving the quality of medical services and patients' health. To reduce the staff fear of the new epidemic, adequate training is required to shed light on the disease's nature and supply adequate resources such as PPE. Furthermore, special attention should be paid to providing HCWs with appropriate levels of social and psychosocial support. In order to improve sleep quality among the staff, the following measures can be taken: decreasing anxiety and depression, applying relaxation techniques, using medications, and providing an opportunity for adequate rest.
Acknowledgement
We appreciate Hamide Behroueian for editing the manuscript in terms of its language and readability.
Conflict of interest: None declared.
attachement [PDF 217 KB] (190 Download)
References
1. Akhlaghi Pirposhteh E, Sheibani N, Beheshti A, Bakhshi N, Salehi Sahl Abadi A. Prevalence of Musculoskeletal Disorders and Occupational Stress among Workers of an Engineering Company in Iran during the Covid-19 Pandemic, 2021: A Cross-Sectional Study. J Occup Health Epidemiol 2021; 10(3):183-92. [DOI]
2. Dost B, Koksal E, Terzi O, Bilgin S, Ustun YB, Arslan HN. Attitudes of Anesthesiology Specialists and Residents toward Patients Infected with the Novel Coronavirus (COVID-19): A National Survey Study. Surg Infect (Larchmt) 2020; 21(4):350-6. [DOI] [PMID]
3. Mirzabeigi AR, Agha Mohammad Hasani P, Sayadi AR, Safarian M, Parand Afshar S. Assessing Health Anxiety among Healthcare Providers of COVID-19 Patients from March to May 2020, Rafsanjan County, Iran. J Occup Health Epidemiol 2021; 10(1):24-30. [DOI]
4. Bjelajac Ž, Filipović A. Lack of Security Culture in Facing the COVID-19 Pandemic. Cult Polis 2020; 17(42):383-99. [Article]
5. Elbay RY, Kurtulmus A, Arpacioglu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res 2020; 290:113130. [DOI] [PMID] [PMCID]
6. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open 2020; 3(3):e203976. [DOI] [PMID] [PMCID]
7. Lung FW, Lu YC, Chang YY, Shu BC. Mental Symptoms in Different Health Professionals During the SARS Attack: A Follow-up Study. Psychiatr Q 2009; 80(2):107-16. [DOI] [PMID]
8. Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020; 7(3):228-9. [DOI] [PMID] [PMCID]
9. Yang X, Chen D, Chen Y, Wang N, Lyv C, Li Y, et al. Geographical distribution and prevalence of mental disorders among healthcare workers in China: A cross-sectional country-wide survey: A cross-sectional study to assess mental disorders of healthcare workers in China. Int J Health Plann Manage 2021; 36(5):1561-74. [DOI] [PMID]
10. Gilleen J, Santaolalla A, Valdearenas L, Salice C, Fusté M. Impact of the COVID-19 pandemic on the mental health and well-being of UK healthcare workers. BJPsych Open 2021; 7(3):e88. [DOI] [PMID] [PMCID]
11. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009; 339:b2700. [DOI] [PMID] [PMCID]
12. Luchini C, Stubbs B, Solmi M, Veronese N. Assessing the quality of studies in meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale. World J Metaanal 2017; 5(4):80-4. [DOI]
13. Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health 2014; 72(1):39. [DOI] [PMID] [PMCID]
14. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21(11):1539-58. [DOI] [PMID]
15. Hunter JP, Saratzis A, Sutton AJ, Boucher RH, Sayers RD, Bown MJ. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J Clin Epidemiol 2014; 67(8):897-903. [DOI] [PMID]
16. Ahmed MA, Jouhar R, Ahmed N, Adnan S, Aftab M, Zafar MS, et al. Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int J Environ Res Public Health 2020; 17(8):2821. [DOI] [PMID] [PMCID]
17. Alshekaili M, Hassan W, Al Said N, Al sulimani F, Jayapal SK, Al-Mawali A, et al. Factors Associated with mental health outcomes across healthcare settings in oman during COVID-19: frontline versus non-frontline healthcare workers. BMJ Open 2020; 10(10):e042030. [DOI] [PubMed] [PMCID]
18. Amerio A, Bianchi D, Santi F, Costantini L, Odone A, Signorelli C, et al. Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Biomed 2020; 91(2):83-8. [DOI] [PMID] [PMCID]
19. An Y, Yang Y, Wang A, Li Y, Zhang Q, Cheung T, et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord 2020; 276:312-5. [DOI] [PMID] [PMCID]
20. Apisarnthanarak A, Apisarnthanarak P, Siripraparat C, Saengaram P, Leeprechanon N, Weber DJ. Impact of anxiety and fear for Covid-19 toward infection control practices among Thai healthcare workers. Infect Control and Hosp Epidemiol 2020; 41(9):1093-4. [DOI] [PMID] [PMCID]
21. Bachilo EV, Barylnik JB, Shuldyakov AA, Efremov AA, Novikov DE. Mental Health of Medical Workers During the COVID-19 Pandemic in Russia: Results of a Cross-Sectional Study. medRxiv 2020. doi: 10.1101/2020.07.27.20162610. [DOI]
22. Badahdah A, Khamis F, Al Mahyijari N, Al Balushi M, Al Hatmi H, Al Salmi I, et al. The mental health of health care workers in Oman during the COVID-19 pandemic. Int J Soc Psychiatry 2021; 67(1):90-5. [DOI] [PMID] [PMCID]
23. Barello S, Palamenghi L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res 2020; 290:113129. [DOI] [PMID] [PMCID]
24. Buselli R, Baldanzi S, Corsi M, Chiumiento M, Del Lupo E, Carmassi C, et al. Psychological Care of Health Workers during the COVID-19 Outbreak in Italy: Preliminary Report of an Occupational Health Department (AOUP) Responsible for Monitoring Hospital Staff Condition. Sustainability 2020; 12(12):5039. [DOI]
25. Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, et al. Psychological Impact and Coping Strategies of Frontline Medical Staff in Hunan between January and March 2020 during the Outbreak of Coronavirus Disease 2019 (COVID) in Hubei, China. Med Sci Monit 2020; 26:e924171. [DOI] [PMID] [PMCID]
26. Çalişkan F, Dost B. The Evaluation of Knowledge, Attitudes, Depression and Anxiety Levels among Emergency Physicians during the COVID-19 Pandemic. Signa Vitae 2020; 16(1):163-71. [DOI]
27. Cao J, Duan Y, Wei J, Zhu H, Geng W, Fritzsche K, et al. The Sooner, the Better: Experience of Early-On Psychological Service to Medical Workers in Fever Clinic of a Tertiary General Hospital in Beijing During COVID-19 Outbreak. 2020. doi: 10.2139/ssrn.3588536. [DOI]
28. Chatterjee SS, Bhattacharyya R, Bhattacharyya S, Gupta S, Das S, Banerjee BB. Attitude, practice, behavior, and mental health impact of COVID-19 on doctors. Indian J Psychiatry 2020; 62(3):257-65. [DOI] [PMID] [PMCID]
29. Chen J, Liu X, Wang D, Jin Y, He M, Ma Y, et al. Multiple Risk Factors of Depression and Anxiety in Medical Staffs: A Cross-Sectional Study at the Outbreak of SARS-CoV-2 in China. 2020. doi: 10.2139/ssrn.3551414 [DOI]
30. Chen X, Zhang SX, Jahanshahi AA, Alvarez-Risco A, Dai H, Li J, et al. Belief in a COVID-19 Conspiracy Theory as a Predictor of Mental Health and Well-Being of Health Care Workers in Ecuador: Cross-Sectional Survey Study. JMIR Public Health Surveill 2020; 6(3):e20737. [DOI] [PMID] [PMCID]
31. Cheng FF, Zhan SH, Xie AW, Cai SZ, Hui L, Kong XX, et al. Anxiety in Chinese pediatric medical staff during the outbreak of Coronavirus Disease 2019: a cross-sectional study. Transl Pediatr 2020; 9(3):231-6. [DOI] [PMID] [PMCID]
32. 35. Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain, Behav Immun 2020; 88:559-65. [DOI] [PMID] [PMCID]
33. Civantos AM, Byrnes Y, Chang C, Prasad A, Chorath K, Poonia SK, et al. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: National study. Head Neck 2020; 42(7):1597-609. [DOI] [PMID] [PMCID]
34. Consolo U, Bellini P, Bencivenni D, Iani C, Checchi V. Epidemiological Aspects and Psychological Reactions to COVID-19 of Dental Practitioners in the Northern Italy Districts of Modena and Reggio Emilia. Int J Environ Res Public Health 2020; 17(10):3459. [DOI] [PMID] [PMCID]
35. Croll L, Kurzweil A, Hasanaj L, Serrano L, Balcer LJ, Galetta SL. The psychosocial implications of COVID-19 for a neurology program in a pandemic epicenter. J Neurol Sci 2020; 416:117034. [DOI] [PMID] [PMCID]
36. Dal'Bosco EB, Floriano LSM, Skupien SV, Arcaro G, Martins AR, Anselmo ACC. Mental health of nursing in coping with COVID-19 at a regional university hospital. Rev Bras Enferm 2020; 73 Suppl 2:e20200434. [DOI] [PMID]
37. Dong ZQ, Ma J, Hao YN, Shen XL, Liu F, Gao Y, et al. The social psychological impact of the COVID-19 pandemic on medical staff in China: A cross-sectional study. Eur Psychiatry 2020; 63(1):e65. [DOI] [PMID] [PMCID]
38. Elbay RY, Kurtulmuş A, Arpacıoğlu S, Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res 2020; 290:113130. [DOI] [PMID] [PMCID]
39. Giusti EM, Pedroli E, D'Aniello GE, Stramba Badiale C, Pietrabissa G, Manna C, et al. The Psychological Impact of the COVID-19 Outbreak on Health Professionals: A Cross-Sectional Study. Front Psychol 2020; 11:1684. [DOI] [PMID] [PMCID]
40. Guo J, Liao L, Wang B, Li X, Guo L, Tong Z, et al. Psychological Effects of COVID-19 on Hospital Staff: A National Cross-Sectional Survey of China Mainland. 2020. doi: 10.2139/ssrn.3550050 [DOI]
41. Hassannia L, Taghizadeh F, Moosazadeh M, Zarghami M, Taghizadeh H, Dooki AF, et al. Anxiety and Depression in Health Workers and General Population During COVID-19 in IRAN: A Cross-Sectional Study. Neuropsychopharmacol Rep 2021; 41(1):40-9. [DOI] [PMID] [PMCID]
42. He JP, Liao R, Yang Y, Li Jj, Weng Nn, Luo Yt, et al. The Research of Mental Health Status among Medical Personnel in China: A Cross-Sectional Study. 2020. doi: 10.2139/ssrn.3555260 [DOI]
43. Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in wuhan, china: a big-scale cross-sectional study. EClinicalMedicine 2020; 24:100424. [DOI] [PMID] [PMCID]
44. Huang L, Wang Y, Liu J, Ye P, Chen X, Xu H, et al. Factors Influencing Anxiety of Health Care Workers in the Radiology Department with High Exposure Risk to COVID-19. Med Sci Monit 2020; 26:e926008. [DOI] [PMID] [PMCID]
45. Kaveh M, Davari-tanha F, Varaei S, Shirali E, Shokouhi N, Nazemi P, et al. Anxiety levels among Iranian health care workers during the COVID-19 surge: A cross-sectional study. MedRxiv 2020. doi: 10.1101/2020.05.02.20089045 [DOI]
46. Labrague LJ, De Los Santos JAA. COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J Nurs Manag 2020; 28(7):1653-61. [DOI] [PMID] [PMCID]
47. Lin Z, Zhang K, He X, Huang Z, Ye W, Ju W, et al. Psychological Burden in Health Care Professionals in Chinese Cities During the Coronavirus Disease 2019 (COVID-19) Outbreak. 2020. doi: 10.2139/ssrn.3576782 [DOI]
48. Liu CY, Yang YZ, Zhang XM, Xu X, Dou QL, Zhang WW, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol Infect 2020; 148:e98. [DOI] [PMID] [PMCID]
49. Liu S, Han W, Shen C, Zhu C, Wang Q, Liang X, et al. The Prevalence and Influencing Factors for Depression Symptom Among Frontline Heathcare Workers from Emergency Department Fighting Against COVID-19: A National Cross-Sectional Survey in China. 2020. doi: 10.2139/ssrn.3588525 [DOI]
50. Liu Z, Han B, Jiang R, Huang Y, Ma C, Wen J, et al. Mental Health Status of Doctors and Nurses during COVID-19 Epidemic in China. 2020. doi: 10.2139/ssrn.3551329 . [DOI]
51. Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res 2020; 288:112936. [DOI] [PMID] [PMCID]
52. Ma Y, Rosenheck R, He H. Psychological stress among health care professionals during the 2019 novel coronavirus disease Outbreak: Cases from online consulting customers. Intensive Crit Care Nurs 2020; 61:102905. [DOI] [PMID] [PMCID]
53. Magnavita N, Tripepi G, Di Prinzio RR. Symptoms in Health Care Workers during the Covid-19 Epidemic. A Cross-Sectional Survey. Int J Environ Res Public Health 2020; 17(14):5218. [DOI] [PMID] [PMCID]
54. Mahendran K, Patel S, Sproat C. Psychosocial effects of the COVID-19 pandemic on staff in a dental teaching hospital. Br Dent J 2020; 229(2):127-32. [DOI] [PMID] [PMCID]
55. Naser AY, Dahmash EZ, Al-Rousan R, Alwafi H, Alrawashdeh HM, Ghoul I, et al. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: A cross-sectional study. Brain Behav 2020; 10(8):e01730. [DOI] [PMID] [PMCID]
56. Qi J, Xu J, Li BZ, Huang JS, Yang Y, Zhang ZT, et al. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep Med 2020; 72:1-4. [DOI] [PMID] [PMCID]
57. Que J, Shi L, Deng J, Liu J, Zhang L, Wu S, et al. Psychological impact of the Covid-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr 2020; 33(3):e100259. [DOI] [PMID] [PMCID]
58. Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, et al. Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw Open 2020; 3(5):e2010185. [DOI] [PMID] [PMCID]
59. Saddik B, Hussein A, Sharif-Askari FS, Kheder W, Temsah MH, Koutaich RA, et al. Increased Levels of Anxiety among Medical And Non-Medical University Students during the Covid-19 Pandemic in the United Arab Emirates. Risk Manag Healthc Policy 2020; 13:2395-406. [DOI] [PMID] [PMCID]
60. Salman M, Raza MH, Mustafa ZU, Khan TM, Asif N, Tahir H, et al. The psychological effects of COVID-19 on frontline healthcare workers and how they are coping: a web-based, cross-sectional study from Pakistan. MedRxiv. 2020. doi: 10.1101/2020.06.03.20119867 [DOI]
61. Sandesh R, Shahid W, Dev K, Mandhan N, Shankar P, Shaikh A, et al. Impact of COVID-19 on the Mental Health of Healthcare Professionals in Pakistan. Cureus 2020; 12(7):e8974. [DOI] [PMID] [PMCID]
62. Savitsky B, Findling Y, Ereli A, Hendel T. Anxiety and coping strategies among nursing students during the covid-19 pandemic. Nurse Educ Pract 2020; 46:102809. [DOI] [PMID] [PMCID]
63. Sögüt S, Dolu İ, Cangöl E. The relationship between COVID-19 knowledge levels and anxiety states of midwifery students during the outbreak: A cross-sectional web-based survey. Perspect Psychiatr Care 2021; 57(1):246-52. [DOI] [PMID] [PMCID]
64. Song X, Fu W, Liu X, Luo Z, Wang R, Zhou N, et al. Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain, Behav Immun 2020; 88:60-5. [DOI] [PMID] [PMCID]
65. Stojanov J, Malobabic M, Stanojevic G, Stevic M, Milosevic V, Stojanov A. Quality of sleep and health-related quality of life among health care professionals treating patients with coronavirus disease-19. Int J Soc Psychiatry 2021; 67(2):175-81. [DOI] [PMID] [PMCID]
66. Sung CW, Chen CH, Fan CY, Su FY, Chang JH, Hung CC, et al. Burnout in Medical Staffs During a Coronavirus Disease (COVID-19) Pandemic. 2020. doi: 10.2139/ssrn.3594567 [DOI]
67. Szepietowski JC, Krajewski P, Biłynicki-Birula R, Poznański P, Krajewska M, Rymaszewska J, et al. Mental health status of health care workers during the COVID-19 outbreak in Poland: One region, two different settings. Dermatol Ther 2020; 33(6):e13855. [DOI] [PubMed] [PMCID]
68. Tan BYQ, Chew NWS, Lee GKH, Jing M, Goh Y, Yeo LLL, et al. Psychological Impact of the COVID-19 Pandemic on Health Care Workers in Singapore. Ann Intern Med 2020; 173(4):317-20. [DOI] [PMID] [PMCID]
69. Temsah MH, Al-Sohime F, Alamro N, Al-Eyadhy A, Al-Hasan K, Jamal A, et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J Infect Public Health 2020; 13(6):877-82. [DOI] [PMID] [PMCID]
70. Teng Z, Wei Z, Qiu Y, Tan Y, Chen J, Tang H, et al. Psychological status and fatigue of frontline staff two months after the COVID-19 pandemic outbreak in China: A cross-sectional study. J Affect Disord 2020; 275:247-52. [DOI] [PMID] [PMCID]
71. Thapa L, Ghimire A, Ghimire S, Sharma N, Shrestha S, Devkota M, et al. Predictors of Anxiety Regarding The COVID-19 Pandemic Among Health-care Workers in a Hospital Not Assigned to Manage COVID-19 Patients in Nepal. MedRxiv 2020. doi: 10.1101/2020.07.08.20148866. [DOI]
72. Vafaei H, Roozmeh S, Hessami K, Kasraeian M, Asadi N, Faraji A, et al. Obstetrics Healthcare Providers’ Mental Health and Quality of Life during Covid-19 Pandemic: Multicenter Study from Eight Cities in Iran. Psychol Res Behav Manag 2020; 13:563-71. [DOI] [PMID] [PMCID]
73. Wang H, Huang D, Huang H, Zhang J, Guo L, Liu Y, et al. The psychological impact of COVID-19 pandemic on medical staff in Guangdong, China: a cross-sectional study. Psychol Med 2022; 52(5):884-92. [DOI] [PMID] [PMCID]
74. Weilenmann S, Ernst J, Petry H, Pfaltz MC, Sazpinar O, Gehrke S, et al. Health Care Worker s' Mental Health during the First Weeks of the SARS-CoV-2 Pandemic in Switzerland: A Cross-Sectional Study. Front Psychiatry 2021; 12:594340. [DOI] [PMID] [PMCID]
75. Xiao H, Shu W, Li M, Li Z, Tao F, Wu X, et al. Social Distancing among Medical Students during the 2019 Coronavirus Disease Pandemic in China: Disease Awareness, Anxiety Disorder, Depression, and Behavioral Activities. Int J Environ Res Public Health 2020; 17(14):5047. [DOI] [PMID] [PMCID]
76. Xiao X, Zhu X, Fu S, Hu Y, Li X, Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: A multi-center cross-sectional survey investigation. J Affect Disord 2020; 274:405-10. [DOI] [PMID] [PMCID]
77. Xiaoming X, Ming A, Su H, Wo W, Jianmei C, Qi Z, et al. The psychological status of 8817 hospital workers during COVID-19 Epidemic: A cross-sectional study in Chongqing. J Affect Disord 2020; 276:555-61. [DOI] [PMID] [PMCID]
78. Xing J, Sun N, Xu J, Geng S, Li Y. Study of the mental health status of medical personnel dealing with new coronavirus pneumonia. PLoS One 2020; 15(5):e0233145. [DOI] [PMID] [PMCID]
79. Yang S, Kwak SG, Ko EJ, Chang MC. The Mental Health Burden of the Covid-19 Pandemic on Physical Therapists. Int J Environ Res Public Health 2020; 17(10):3723. [DOI] [PMID] [PMCID]
80. Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, et al. Survey of Insomnia and Related Social Psychological Factors among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Front Psychiatry 2020; 11:306. [DOI] [PMID] [PMCID]
81. Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother Psychosom 2020; 89(4):242-50. [DOI] [PMID] [PMCID]
82. Zhu J, Sun L, Zhang L, Wang H, Fan A, Yang B, et al. Prevalence and Influencing Factors of Anxiety and Depression Symptoms in the First-Line Medical Staff Fighting Against COVID-19 in Gansu. Front Psychiatry 2020; 11:386. [DOI] [PMID] [PMCID]
83. Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G, et al. COVID-19 in Wuhan: Sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. EClinicalMedicine 2020; 24:100443. [DOI] [PMID] [PMCID]
84. Marques AA, Bevilaqua MC, da Fonseca AM, Nardi AE, Thuret S, Dias GP. Gender Differences in the Neurobiology of Anxiety: Focus on Adult Hippocampal Neurogenesis. Neural Plast 2016; 2016:5026713. [DOI] [PMID] [PMCID]
85. Remes O, Brayne C, van der Linde R, Lafortune L. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav 2016; 6(7):e00497. [DOI] [PMID] [PMCID]
86. Petzold MB, Bendau A, Plag J, Pyrkosch L, Mascarell Maricic L, Betzler F, et al. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav 2020; 10(9):e01745. [DOI] [PMID] [PMCID]
87. Sheraton M, Deo N, Dutt T, Surani S, Hall-Flavin D, Kashyap R. Psychological effects of the COVID 19 pandemic on healthcare workers globally: A systematic review. Psychiatry Res 2020; 292:113360. [DOI] [PMID] [PMCID]
88. Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, et al. Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. EClinicalMedicine 2020; 24:100424. [DOI] [PMID] [PMCID]
89. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behav Immun 2020; 88:901-7. [DOI] [PMID] [PMCID]
90. Bahrami F, Yousefi N. Females are more anxious than males: a metacognitive perspective. Iran J Psychiatry Behav Sci 2011; 5(2):83-90. [PMID] [PMCID]
91. Jalnapurkar I, Allen M, Pigott T. Sex Differences in Anxiety Disorders: A Review. J Psychiatry Depress Anxiety 2018; 4:012. [DOI]
92. Muller AE, Hafstad EV, Himmels JPW, Smedslund G, Flottorp S, Stensland SØ, et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Res 2020; 293:113441. [DOI] [PMID] [PMCID]
93. da Silva Neto RM, Benjamim CJR, de Medeiros Carvalho PM, Neto MLR. Psychological effects caused by the COVID-19 pandemic in health professionals: A systematic review with meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry 2021; 104:110062. [DOI] [PMID] [PMCID]
94. Choi KW, Kim YK, Jeon HJ. Comorbid Anxiety and Depression: Clinical and Conceptual Consideration and Transdiagnostic Treatment. Adv Exp Med Biol 2020; 1191:219-35. [DOI] [PMID]
95. Seeman MV. Why Are Women Prone to Restless Legs Syndrome? Int J Environ Res Public Health 2020; 17(1):368. [DOI] [PMID] [PMCID]
96. Labaka A, Goni-Balentziaga O, Lebena A, Perez-Tejada J. Biological Sex Differences in Depression: A Systematic Review. Biol Res Nurs 2018; 20(4):383-92. [DOI] [PMID]
97. Morin CM, Drake CL, Harvey AG, Krystal AD, Manber R, Riemann D, et al. Insomnia disorder. Nat Rev Dis Primers 2015; 1:15026. [DOI] [PMID]
98. Jansson M, Rello J. Mental Health in Healthcare Workers and the Covid-19 Pandemic Era: Novel Challenge for Critical Care. J Intensive Crit Care 2020; 6(2:6). doi: 10.36648/2471-8505.6.2.6 [Article]
99. Qiu D, Yu Y, Li RQ, Li YL, Xiao SY. Prevalence of sleep disturbances in Chinese healthcare professionals: a systematic review and meta-analysis. Sleep Med 2020; 67:258-66. [DOI] [PMID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution 4.0 International License. |








